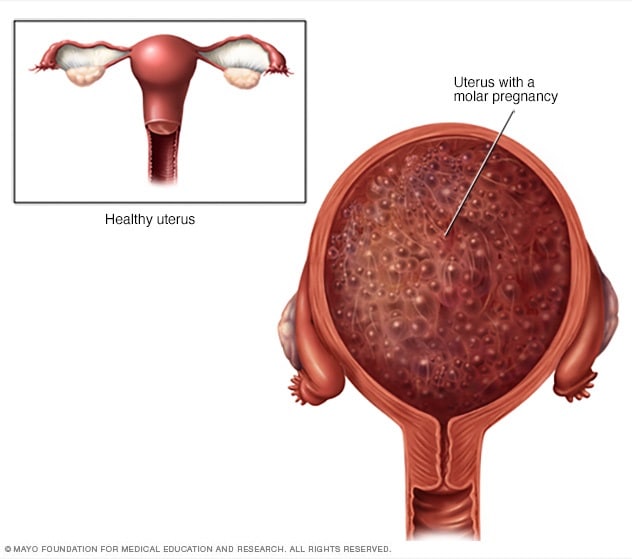
A molar pregnancy — also known as hydatidiform mole — is a rare complication of pregnancy characterized by the abnormal growth of trophoblasts, the cells that normally develop into the placenta.
There are two types of molar pregnancy, complete molar pregnancy and partial molar pregnancy. In a complete molar pregnancy, the placental tissue is abnormal and swollen and appears to form fluid-filled cysts. There’s also no formation of fetal tissue. In a partial molar pregnancy, there may be normal placental tissue along with abnormally forming placental tissue. There may also be formation of a fetus, but the fetus is not able to survive, and is usually miscarried early in the pregnancy.
A molar pregnancy can have serious complications — including a rare form of cancer — and requires early treatment.
Symptoms
A molar pregnancy may seem like a normal pregnancy at first, but most molar pregnancies cause specific signs and symptoms, including:
- Dark brown to bright red vaginal bleeding during the first trimester
- Severe nausea and vomiting
- Sometimes vaginal passage of grapelike cysts
- Pelvic pressure or pain
If you experience any signs or symptoms of a molar pregnancy, consult your doctor or pregnancy care provider. He or she may detect other signs of a molar pregnancy, such as:
- Rapid uterine growth — the uterus is too large for the stage of pregnancy
- High blood pressure
- Preeclampsia — a condition that causes high blood pressure and protein in the urine after 20 weeks of pregnancy
- Ovarian cysts
- Anemia
- Overactive thyroid (hyperthyroidism)
Causes
A molar pregnancy is caused by an abnormally fertilized egg. Human cells normally contain 23 pairs of chromosomes. One chromosome in each pair comes from the father, the other from the mother.
In a complete molar pregnancy, an empty egg is fertilized by one or two sperm, and all of the genetic material is from the father. In this situation, the chromosomes from the mother’s egg are lost or inactivated and the father’s chromosomes are duplicated.
In a partial or incomplete molar pregnancy, the mother’s chromosomes remain but the father provides two sets of chromosomes. As a result, the embryo has 69 chromosomes instead of 46. This most often occurs when two sperm fertilize an egg, resulting in an extra copy of the father’s genetic material.
Risk factors
Approximately 1 in every 1,000 pregnancies is diagnosed as a molar pregnancy. Various factors are associated with molar pregnancy, including:
- Maternal age. A molar pregnancy is more likely in women older than age 35 or younger than age 20.
- Previous molar pregnancy. If you’ve had one molar pregnancy, you’re more likely to have another. A repeat molar pregnancy happens, on average, in 1 out of every 100 women.
Complications
After a molar pregnancy has been removed, molar tissue may remain and continue to grow. This is called persistent gestational trophoblastic neoplasia (GTN). This occurs in approximately 15 to 20 percent of complete molar pregnancies, and up to 5 percent of partial molar pregnancies.
One sign of persistent GTN is a high level of human chorionic gonadotropin (HCG) — a pregnancy hormone — after the molar pregnancy has been removed. In some cases, an invasive hydatidiform mole penetrates deep into the middle layer of the uterine wall, which causes vaginal bleeding.
Persistent GTN can nearly always be successfully treated, most often with chemotherapy. Another treatment option is removal of the uterus (hysterectomy).
Rarely, a cancerous form of GTN known as choriocarcinoma develops and spreads to other organs. Choriocarcinoma is usually successfully treated with multiple cancer drugs. A complete molar pregnancy is more likely to have this complication than a partial molar pregnancy.
Prevention
If you’ve had a molar pregnancy, talk to your doctor or pregnancy care provider before conceiving again. He or she may recommend waiting for six months to one year before trying to become pregnant. The risk of recurrence is low, but higher than the risk for women with no previous history of molar pregnancy.
During any subsequent pregnancies, your care provider may do early ultrasounds to monitor your condition and offer reassurance of normal development. Your provider may also discuss prenatal genetic testing, which can be used to diagnose a molar pregnancy.